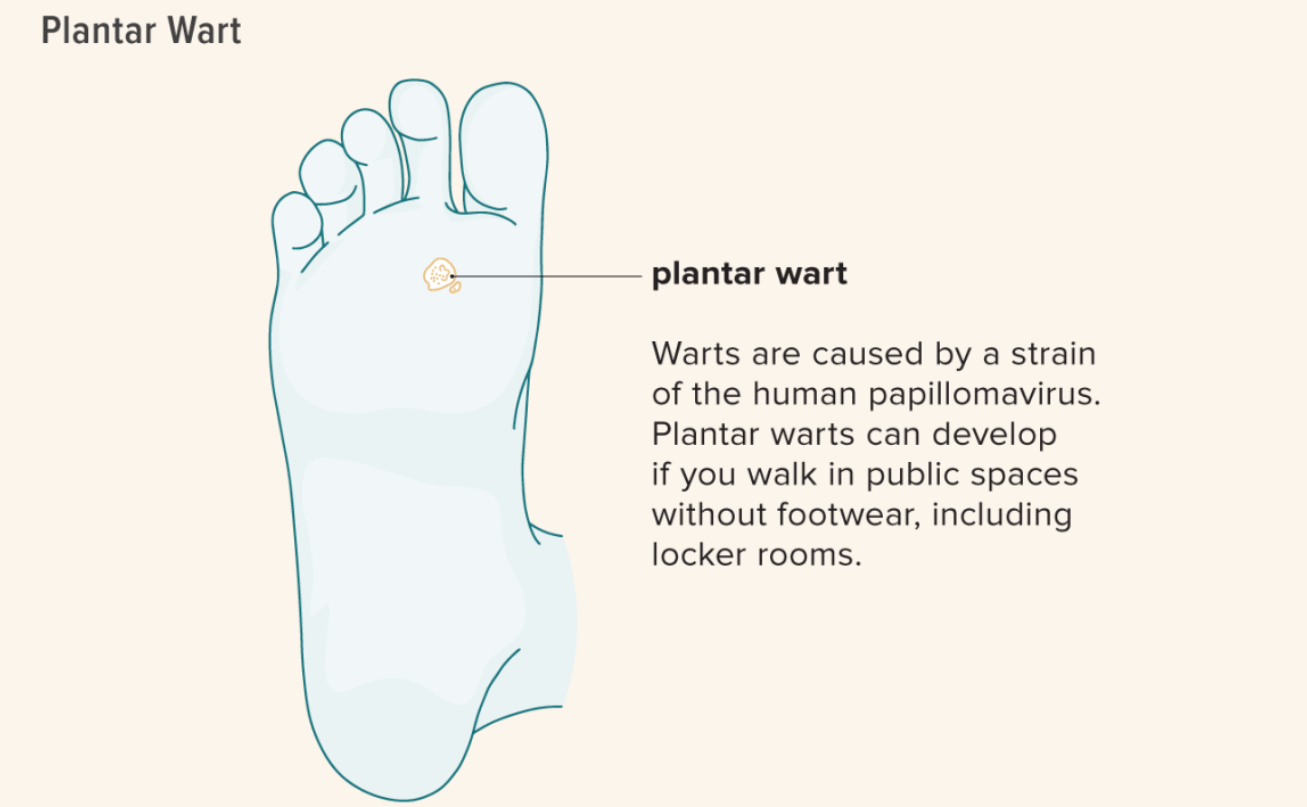
Ever feel a sharp pain with every step? Plantar warts, those pesky growths on your feet, can be a real pain (literally!). But fear not, fellow foot warriors! This guide will reveal the top 6 home remedies dermatologists recommend to…
Call Us Now
0207 030 3370
Lines Open: 9am – 9pm | Mon – SunAward Winning
5-Star Rated Clinic
5/5