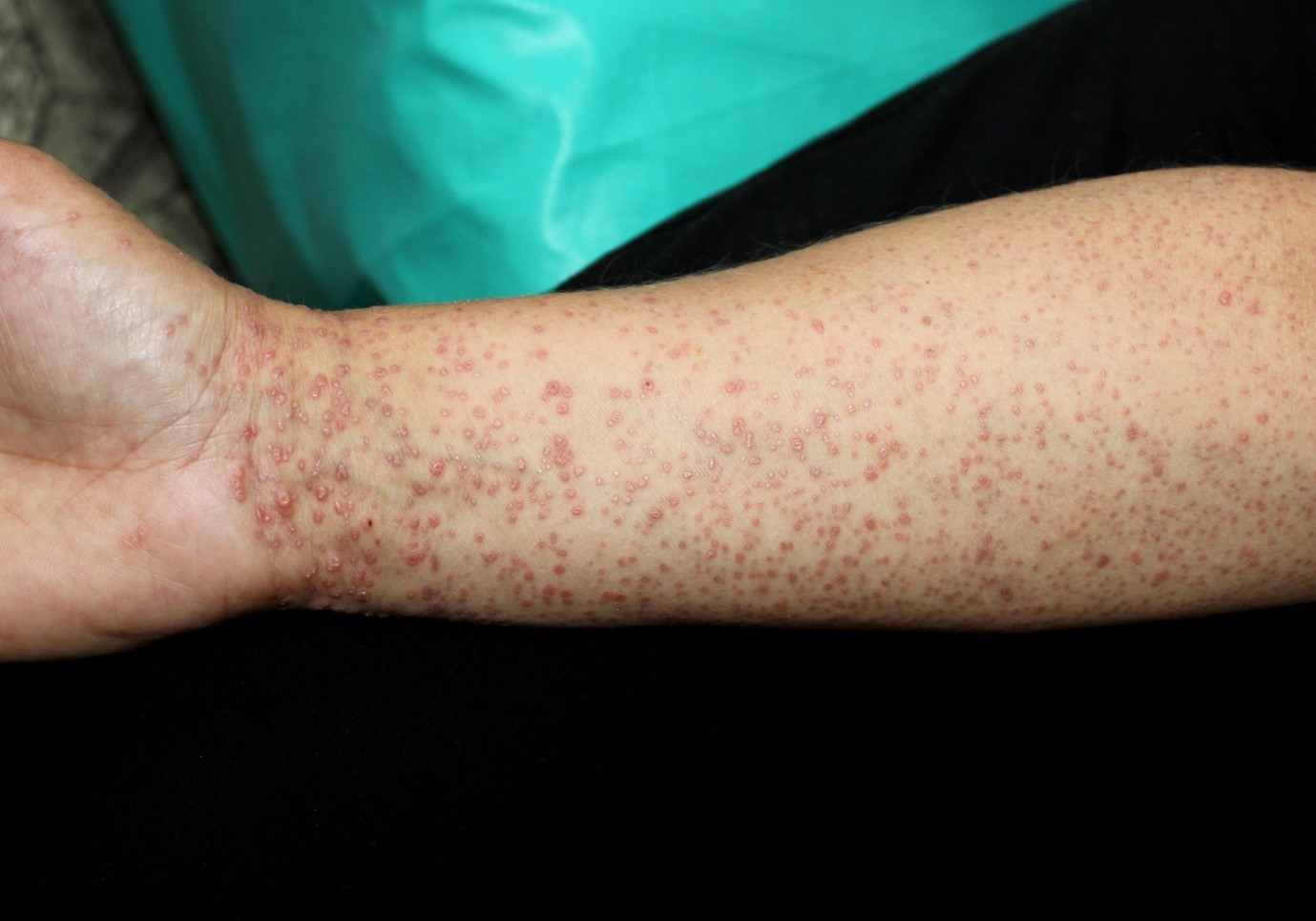
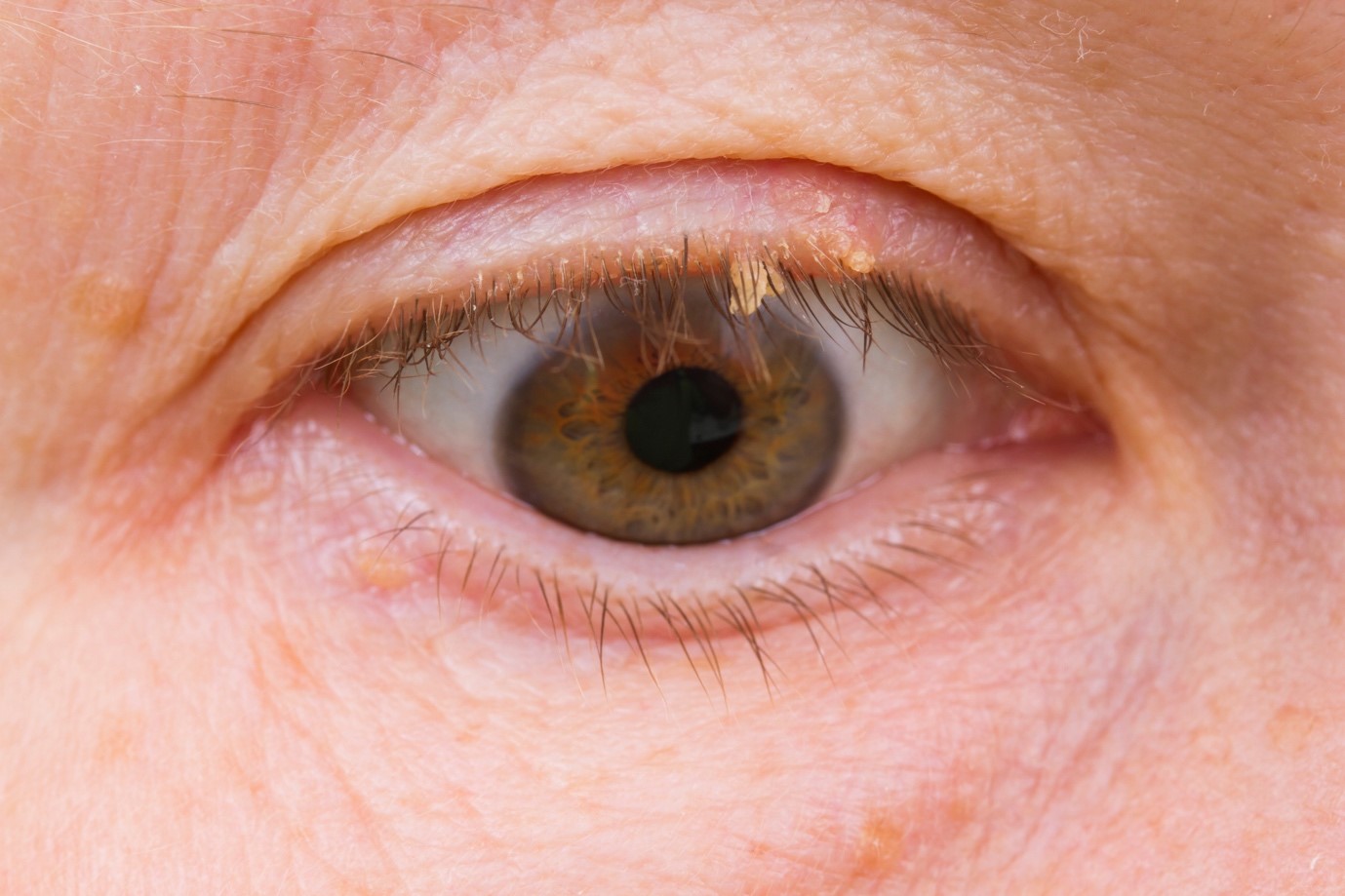
Discover comprehensive Lichen Planus treatment options, how to get an expert diagnosis and tailored therapies for effective relief. Lichen Planus Treatment is crucial when managing this chronic inflammatory skin condition. In this blog post, we will delve into understanding Lichen…
Call Us Now
0207 030 3370
Lines Open: 9am – 9pm | Mon – SunAward Winning
5-Star Rated Clinic
5/5